An innovative skin patch developed by researchers at the Leslie Dan Faculty of Pharmacy has the potential to prevent low blood sugar levels (hypoglycemia) in people with diabetes. Shirley Wu and her team designed a “smart” patch that delivers the hormone glucagon to the bloodstream in response to hypoglycemia, thus preventing the dangerous condition.
A considerable number of people with diabetes need to administer insulin to manage their high blood glucose levels. But intensive insulin therapy may often lead to hypoglycemia, causing sweating, shaking, confusion, seizures and even death. Currently, episodes of severe hypoglycemia are treated with an emergency injection or nasal spray of glucagon formulation, but people with diabetes or their caregivers need to recognize the symptoms and deliver an emergency treatment quickly. This is a big challenge for people with hypoglycemia unawareness or who are unable to handle the complex treatment procedures.
“Our microneedle patch is the first of its kind"
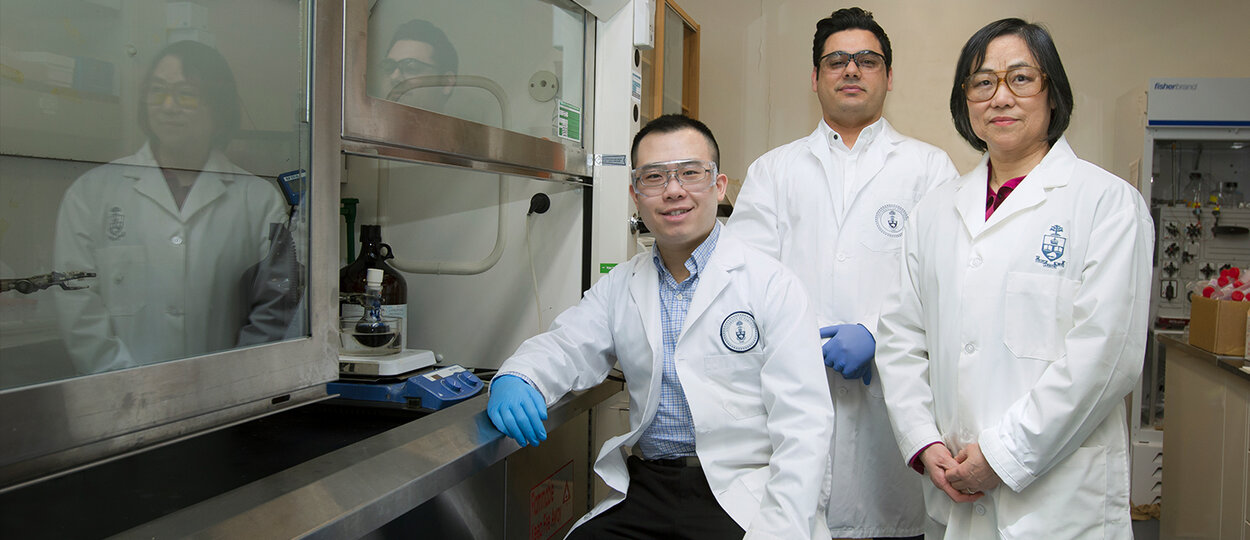
With funding from the JDRF, Shirley Wu, a professor at the Faculty who studies drug delivery systems, and her team developed a disposable, one-time use patch that can currently prevent the condition in animal models. “Our microneedle patch is the first of its kind. No other microneedle patch is responsive to low glucose concentration. Ours is sensitive enough to detect hypoglycemia and release glucagon when it’s needed,” she says.
‘Smart’ design releases glucagon automatically
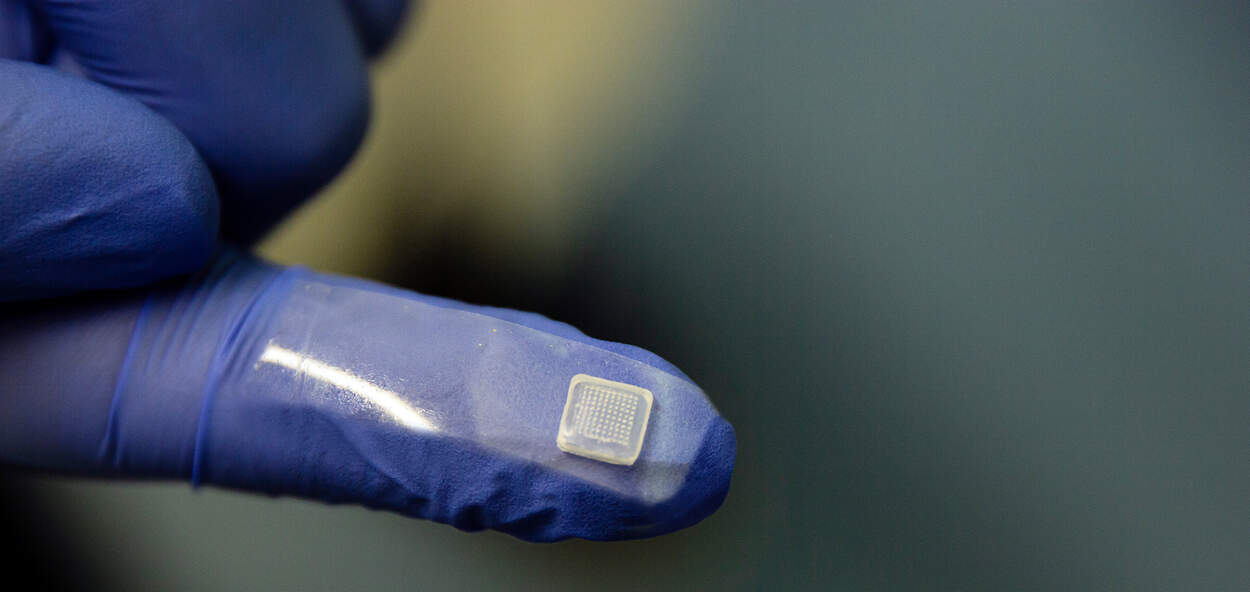
The microneedle patch looks like a nicotine patch, but it features an array of one hundred tiny needles less than a millimetre long. “The tiny needles penetrate the first layer of the skin allowing access to interstitial fluid to sense glucose levels, but they don’t reach any pain sensors, so the patch application is painless and minimally-invasive,” says Amin GhavamiNejad, a post-doctoral fellow in the Wu lab.
The microneedles contain a sponge-like microgel loaded with glucagon. One of the microgel components bonds with glucose, blocking glucagon from being released into the blood at high or normal blood sugar levels. But when blood sugar level is low, glucose separates from the microgel causing the microgel to shrink, which physically squeezes the encapsulated glucagon into the tissue rapidly through the microneedles.
“It circumvents the need for patients or caregivers to recognize the symptoms of hypoglycemia, since it senses the episode and takes care of it automatically,” says Brian Lu, a PhD student in the Wu lab. “This smart design is what makes the patch unique and novel.”
Glucagon is highly unstable, and designing the microgel system so that it could hold glucagon without altering it was a feat in itself. In a paper published in the journal Advanced Materials in 2019, they demonstrated that the patch was successfully loaded with glucagon and that the patch released glucagon in an animal model in response to low blood glucose level, preventing hypoglycemia for up to three hours. The animal studies have been performed in collaboration with Prof. Adria Giacca’s lab from the Faculty of Medicine at U of T.
Team motivated to bring technology to patients
Since the team published the research several months ago, a number of people with diabetes and caregivers have asked when the patch will be tested in clinical trials. More research needs to be done before trials can begin, but the team is excited about the potential of this innovative technology to transform diabetes treatment and care. And the enormous interest from the community motivates them to move the research forward. “Our goal is to benefit patients,” says Wu. “We need to work harder and faster to move this technology to the community.”
“At U of T, we have access to everything we need to conduct innovative research”
Wu says that being based at U of T and in the Leslie Dan Faculty of Pharmacy has been crucial to her group’s work – she has developed collaborations with other researchers and clinicians, received support for technology development and IP protection and received funding from the Banting and Best Diabetes Centre, in addition to JDRF. “At U of T, we have access to everything we need to conduct innovative research,” she says.
GhavamiNejad agrees. “It’s a great environment in the laboratory and in this top university,” he says. “It’s the perfect setting for a group that wants to develop something new that can help patients.”
By: Eileen Hoftyzer
More News
Image
Grad to Watch: Jackie Fule Liu’s research focuses on better outcomes for diabetes patients
A recent PhD graduate, Jackie Fule Liu combines hands-on skill and big-picture thinking to help tackle diabetes care challenges.
Read More
Image

U of T community members recognized with Order of Canada
Congratulations to Dean Emeritus and Professor K. Wayne Hindmarsh on his appointment.
Read More
Image

Welcoming Ivy Lam as Academic Lead in Climate, Health & Sustainable Care
Assistant Professor Lam will guide the Leslie Dan Faculty of Pharmacy's efforts to embed environmental sustainability across the Faculty.
Read More