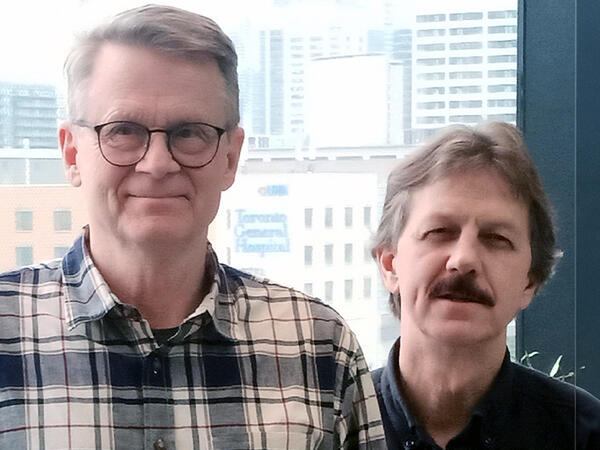
From left: Pharmacist and pharmaceutical sciences masters student Timothy Lim, assistant professor Jaris Swidrovich
Jaris Swidrovich will explore barriers to accessing HIV prevention drug and how health care providers can provide better care to Indigenous Peoples
Working in inpatient HIV care in Saskatoon, Jaris Swidrovich saw firsthand the disproportionate impact that human immunodeficiency virus (HIV) has on Indigenous Peoples in Canada.
The historical and ongoing impacts of colonialism – including anti-Indigenous racism, intergenerational trauma, and government policies that have disadvantaged Indigenous Peoples – have resulted in Indigenous Peoples in Canada experiencing poorer health outcomes than non-Indigenous Canadians.
When it comes to HIV, the statistics are staggering. In 2020, the Public Health Agency of Canada reported that the national rate of HIV cases was 4.3 new infections per 100,000 people, but the rate for Indigenous Peoples was 15.2 new infections per 100,000 people.
And while many people in Canada at higher risk of HIV are able to access highly effective preventive care with pre-exposure prophylaxis (PrEP), Indigenous Peoples face more barriers in getting the care they need.
“Working in Saskatoon, almost all of the patients I saw in the inpatient environment were Indigenous. And if they had all been on PrEP for their lives, that would have been a very different story,” says Swidrovich, assistant professor (teaching stream) and Indigenous Engagement Lead at the Leslie Dan Faculty of Pharmacy.
PrEP is a preventive medication that people without HIV can take to lower their risk of acquiring HIV.
Research has shown that it is 99 per cent effective in preventing sexual transmission of HIV, and between 70 per cent and 80 per cent effective at preventing HIV transmission through using injection drugs.
After moving to Toronto, Swidrovich heard from other HIV pharmacists and Indigenous community members that, in their experiences, few Indigenous Peoples knew about PrEP and how to access it. And the very little research that has been done on PrEP use among Indigenous Peoples has suggested that uptake is very low.
“There is some literature about PrEP uptake, but it’s not specific to Indigenous Peoples, and the factors that influence uptake in other groups may not apply to Indigenous Peoples,” says Swidrovich. “We don’t know the reasons for the lack of uptake in urban Indigenous Peoples.”
To explore this question, Swidrovich recently received a nearly $100,000 CIHR Catalyst Grant to explore the barriers to PrEP use that urban Indigenous Peoples face as well as facilitators and opportunities to improve knowledge and uptake.
Swidrovich has partnered with community organizations in the Greater Toronto Area, including the 2-Spirited Peoples of the 1st Nations and Toronto Indigenous Harm Reduction, to host Talking Circles with Indigenous Peoples who have a higher risk of acquiring HIV, either through sexual transmission or injection drug use.
Using Indigenous methodologies, which prioritize conversations, relationships, and storytelling, the research team will learn from the participants about their knowledge about and experiences with PrEP, barriers they have faced to accessing PrEP, and how health care providers can improve access to PrEP for Indigenous Peoples.
“In addition to helping us understand current barriers that exist around PrEP use, access and adherence, the study is also an opportunity for Indigenous Peoples to be a part of health care change,” says Timothy Lim, a pharmacist and master’s student at the Leslie Dan Faculty of Pharmacy working with Swidrovich on the project. “Hopefully the Talking Circles will unravel unique opportunities for pharmacists to improve PrEP access and also help drive policy change that not only improves patient care, but also expands pharmacist scope of practice, for example to prescribe PrEP or order lab values.”
A key part of Indigenous methodology and approach is that research relationships are reciprocal, and the research team gives something back to the community they are researching with. To that end, Swidrovich and Lim are hosting information sessions on health topics and providing one-on-one medication reviews for members of the community organizations.
Once they have results from the study, they also plan to implement them directly in the community and work with pharmacists and community organizations to design approaches to help improve HIV preventive care and PrEP access for Indigenous Peoples.
In the meantime, Swidrovich and Lim say that pharmacists can help improve awareness around PrEP by educating themselves about PrEP, posting information in their pharmacy or clinic, and having conversations and counselling patients who would benefit from this medication, as well as understanding drug coverage for First Nations Peoples and Inuit through the Non-Insured Health Benefits program.
“We want to ensure that any folks who prescribe, suggest, dispense, monitor, or follow patients on PrEP know why they’re not seeing Indigenous folks, or why they are seeing the ones who they are seeing,” Swidrovich says. “Hopefully we can provide some strategies for better knowledge, awareness, and uptake of PrEP.”
More News
Image
Jeffrey Henderson Receives Prestigious Connaught Innovation Award
Award will support research to advance novel method of modifying cells for testing new gene therapies.
Read More
Image

Faces of PharmSci: Mahya Rezaeifarimani
Supervised by Prof. Shirley Wu, PhD student Mahya Rezaeifarimani is developing smart nanoparticles to help make radiation therapy work better for brain tumours by targeting low-oxygen areas that often make treatment less effective.
Read More
Image

Dean Lisa Dolovich reappointed for second term
Professor Lisa Dolovich has been reappointed for a second term as Dean of the Leslie Dan Faculty of Pharmacy, University of Toronto, effective July 1, 2025, to December 30, 2030.
Read More
