Medications improve health and saves lives, but they are not risk-free. The modern pharmacist is largely responsible for helping patients navigate an increasingly complex and costly health care system, particularly with respect to medications. And with significant changes in population demographics, technology, and the upsurge in the use of health services across the sector, a group of pharmacist-researchers from the Ontario Pharmacy Evidence Network is calling for the profession to make fundamental changes to effectively and safely meet society's health care needs.
An overview of these recommendations is captured in a peer-reviewed paper published earlier this month in the Canadian Pharmacists Journal (CPJ/RPC).
"Patients, families and other health care providers rely on pharmacists to support safe and effective medication use and we need to think seriously about how we can shift and adapt our practice to meet changing health care trends," says lead author Lisa Dolovich, professor at the Leslie Dan Faculty of Pharmacy, University of Toronto. "We feel that transformational change in the profession of pharmacy is essential in all practice settings including community, hospital, primary care or other organizations."
For example, in the future, dispensing medication may not be a significant component of on-site pharmacy services, the authors write. Recognizing that dispensing and front-store products are increasingly managed by off-site storage and delivery, pharmacies should look to repurpose physical layout and optimize workflow processes to better support patient assessment and communication, including the use of eHealth technology, private rooms and interprofessional teamwork.
"This type of organizational-level change will better support pharmacists' ability to be integrated into a patient's overall care plan, more effectively work with other primary care providers and open opportunities for pharmacists to expand disease monitoring and prevention services," says Nancy Waite, professor and associate director of clinical education at University of Waterloo's School of Pharmacy.
Pharmacists, particularly those who work in the community, are also well positioned to support better integration of patient care across the health care system. But this requires better use of technology to collaborate with other care providers and with pharmacists in other care settings, the authors write. In the future, pharmacists should be able to easily triage or refer patients to other health and community organizations and also have a system in place to receive referrals. Pharmacists should have access to and interpret clinical information from other services including lab and diagnostic test results.
The authors note that in many recent policy discussions about the future direction of health care services, the voice of pharmacists has been largely absent. This is surprising given total drug spending in Canada was estimated to be $39.8 billion in 2017 and made up the second largest share of health care expenditures.
"Pharmacists are an under-utilized resource in health care and we see opportunities for pharmacists to really become a patient's partner in preventing and managing illness, improving transitions between different levels of care, as well as their medication use," says Dolovich. "There is much more pharmacists can do to help build an integrated care system that is centred on individual patients' needs, within their community, and throughout every stage of life."
The research was supported by the Ontario College of Pharmacists and Ontario Pharmacy Evidence Network. The paper published in CPJ is a condensed and adapted version of a White Paper prepared by the Ontario Pharmacy Evidence Network (OPEN) at the request of the Ontario College of Pharmacists (OCP) for the purpose of stimulating a discussion within the profession.
More News
Image
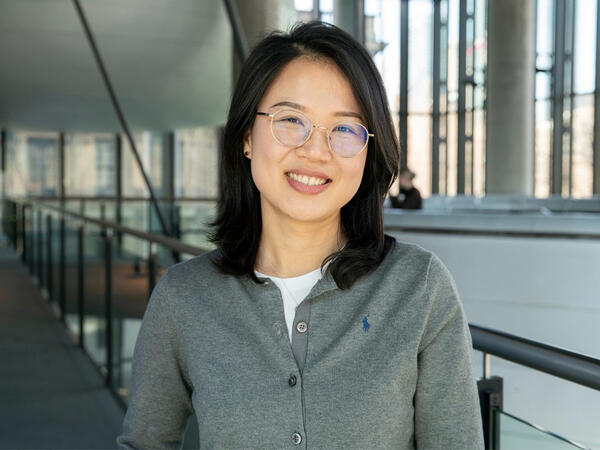
Grad to Watch: Jackie Fule Liu’s research focuses on better outcomes for diabetes patients
A recent PhD graduate, Jackie Fule Liu combines hands-on skill and big-picture thinking to help tackle diabetes care challenges.
Read More
Image

U of T community members recognized with Order of Canada
Congratulations to Dean Emeritus and Professor K. Wayne Hindmarsh on his appointment.
Read More
Image

Welcoming Ivy Lam as Academic Lead in Climate, Health & Sustainable Care
Assistant Professor Lam will guide the Leslie Dan Faculty of Pharmacy's efforts to embed environmental sustainability across the Faculty.
Read More