As many as 1 in 5 Canadians are affected by chronic pain. Yet there has been limited progress on new drug development for the treatment of pain for several decades. Opioids remain one of the most effective medications for treating acute pain, but they work by dampening down symptoms and do little to treat the underlying cause. The now well-known risk of addiction surges after only a few days of use and the “opioid epidemic” – brought on in part by the overprescribing of this powerful class of drugs – has become a widespread problem in North America, resulting in thousands of deaths.
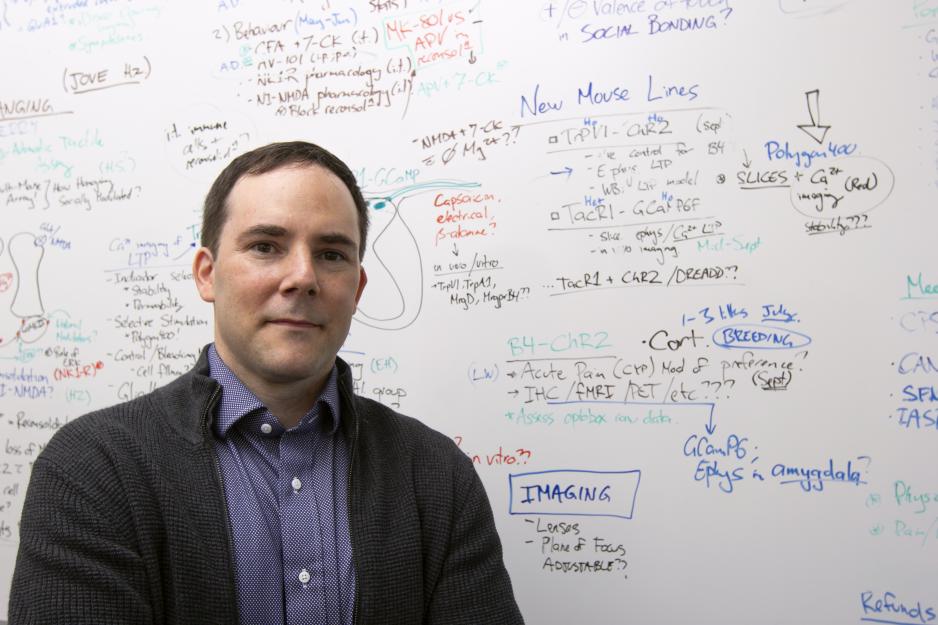
Robert Bonin, assistant professor at the Leslie Dan Faculty of Pharmacy, University of Toronto, and Canada Research Chair in Sensory Plasticity and Reconsolidation, is investigating potential new avenues for treating chronic pain by first looking at how pain arises at the most fundamental level. “We are studying the communication between cells in the spinal cord, to understand how pathological pain operates at the molecular level,” he says.
Chronic, pathological pain occurs when pain associated with an injury or illness persists beyond a normal recovery time and begins to cause intensified pain sensation, which can be debilitating.
“Pain has an important protective function – a sunburn, for example, signals to us that we’ve been exposed to the sun for too long. But in the case of chronic, runaway pain there is no longer any benefit and it can become a serious health issue without any truly effective curative options,” says Bonin. “Essentially, people get stuck in a highly sensitized state and can’t get out of it.”
The downside of brain plasticity
Specifically, professor Bonin and his research team are looking for a new molecular pathway to directly reverse the cellular changes that contribute to pathological pain. Bonin, who runs the Sensory Plasticity lab in the Faculty of Pharmacy, is building on our understanding of how memory works in order to shed light on the roots of chronic pain.
The central nervous system is designed to be plastic, to adapt and learn, but not all changes are good. “Conditions like chronic pain and Post Traumatic Stress Disorder (PTSD) are examples of a maladaptive learning process,” says Bonin. “The stimulus or event that has caused the trauma is over – some times for years – but there remains a highly reactive ‘memory trace’ of the event that can cause pain or distress. We are exploring how to have the nervous system forget this memory trace that contributes to chronic pain”
Retrigger and erase
As a postdoctoral fellow, Bonin worked alongside Yves De Koninck, a professor of neuroscience at Université Laval exploring the physiological parallels between memory and pain. Scientists have proven that memories are not static and that it is possible to retrigger a previously created memory to update, modify, or even erase memories – an approach known as reconsolidation. “We observed that, like memories, experimentally-induced, persistent pathological pain could also be targeted and erased by manipulating reconsolidation.”
In a similar way that psychologists look to reverse the pathological emotional memory of PTSD, Bonin is searching for the underlying mechanisms responsible for creating pain memory traces in an effort to target and then erase these cellular changes. It is not yet clear which signalling pathways are responsible for pathological pain, but Bonin is focused on the NMDA receptor in the spinal pain processing pathways. “We know that this receptor plays an important role in memory functioning and we also believe that it offers a target for pain memory traces,” he says. “If we can selectively target just the pain pathway, leaving the rest of the nervous system intact, it’s possible we could develop medications to actually treat the underlying cause of chronic pain, and provide patients and healthcare providers with more effective options.”
While this work is in early stages and a number of years away from clinical application, the approach is “tantalizingly promising” and offers the possibility of an entirely new approach to treating chronic pain.
More News
Image

Jeffrey Henderson Receives Prestigious Connaught Innovation Award
Award will support research to advance novel method of modifying cells for testing new gene therapies.
Read More
Image

Dean Lisa Dolovich reappointed for second term
Professor Lisa Dolovich has been reappointed for a second term as Dean of the Leslie Dan Faculty of Pharmacy, University of Toronto, effective July 1, 2025, to December 30, 2030.
Read More
Image

Faces of PharmSci: Mahya Rezaeifarimani
Supervised by Prof. Shirley Wu, PhD student Mahya Rezaeifarimani is developing smart nanoparticles to help make radiation therapy work better for brain tumours by targeting low-oxygen areas that often make treatment less effective.
Read More