Pharmacy, dentistry, medicine and nursing experts discussed the complexities, impact and treatment of pain at webinar
An interdisciplinary panel of University of Toronto experts discussed research and clinical advances in pain management at a webinar on November 4.
Pain is a universal phenomenon that health professionals across all disciplines encounter in individuals of all ages, in all health care settings, and across all situations. The Managing Pain webinar brings together health sciences faculty from U of T’s Centre for the Study of Pain (UTCSP).
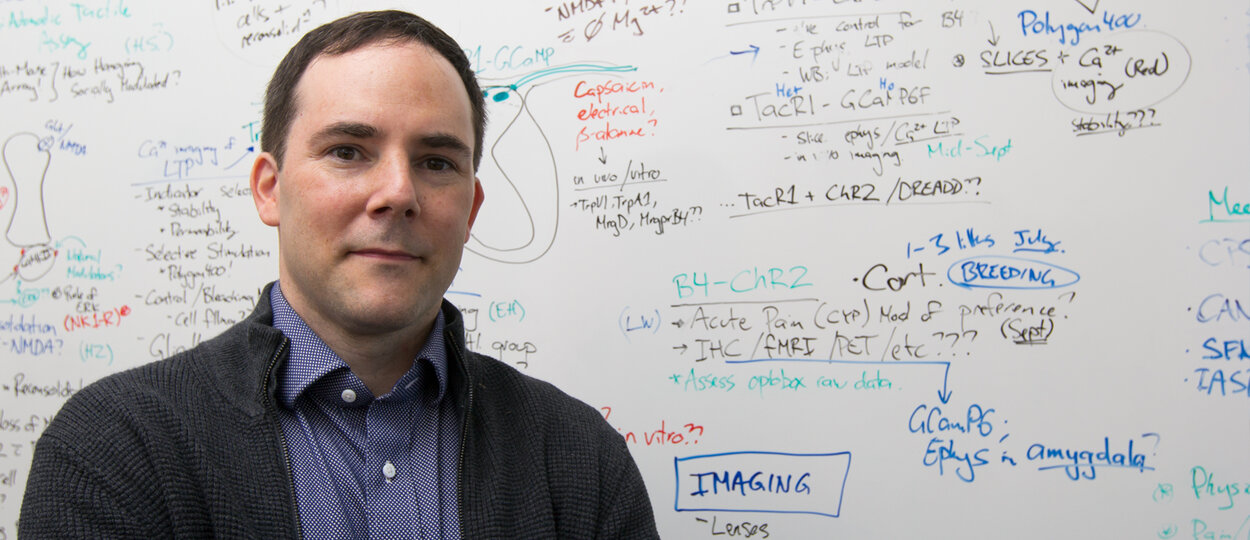
The Centre is co-directed by Dr. Rachael Bosma, Assistant Professor in the Faculty of Dentistry (event moderator), and Dr. Rob Bonin, Assistant Professor in the Leslie Dan Faculty of Pharmacy. They will be joined by fellow panelists Dr. Abhimanyu Sud, Assistant Professor in the Temerty Faculty of Medicine and Monica Parry, Associate Professor in the Lawrence S. Bloomberg Faculty of Nursing.
Watch the full 'Managing Pain' webinar
The Communications Team at the Leslie Dan Faculty of Pharmacy met with Professor Bonin — who also holds the Canada Research Chair in Sensory Plasticity and Reconsolidation — before his talk for a preview of the discussion, his research, and how UTCSP is taking a holistic approach to pain management.
What is pain?
Everyone is familiar with pain. Pain is best described as an experience and cannot be distilled down to a simple process of sensation. This is because pain is not just sensation, it is also emotional and socially relevant and can change our behaviour. In a positive sense, pain serves as an alert to potential or actual injury to keep us safe. It is when that warning signal becomes chronic and outlives its adaptive use that pain becomes debilitating.
But we also all have our own unique understanding of pain, whether it’s how we remember the sting of a vaccine jab or are living with a chronic pain condition.
What makes pain difficult to study (and treat)?
We do have effective treatments for some types of pain. When a dentist freezes your teeth, this local anesthesia can be a highly effective means of preventing acute pain. The difficulty arises in the treatment of chronic pain, where something like ongoing anesthesia for chronic lower back pain is just not practical. One major difficulty is that chronic pain is a complex process that can have many causes. Because pain is an experience, we could look at how the brain processes pain.
As many research groups have shown, including those at the University of Toronto, there is no specific pain centre in the brain that lights up during pain and could possibly be targeted for treatment. Pain can arise from the complex interaction of enhanced activation of pain sensing nerves in the periphery, to altered processing of these sensory signals in the spinal cord, to changes in the processing of all this information in the brain. In some cases of chronic pain there is simply no discernable cause of pain, yet the pain exists and is real.
Historically, pain has been viewed as a symptom of another problem, but it’s increasingly recognized as its own condition requiring concerted research and treatment efforts. In our own research, we are looking at how sensory inputs are sent to the spinal cord, and then processed (or misprocessed) as painful stimuli.
One aspect of this work that has stood out to me is that even in the absence of injury, slight changes in how cells communicate with one another along the pain processing pathway can lead to pathological pain. We are working to better understand how changes can occur along the entire “pain connectome”, and how to address these changes.
Why are we at a “critical juncture” in the translation of pain research into practice?
Chronic pain is increasing in prevalence globally, in part because people are living longer and having more medical procedures that can result in chronic pain. People are also having more age-related diseases that contribute to chronic pain, and perhaps counter-intuitively, improvements in cancer treatment can themselves lead to chronic pain.
Because the prevalence of chronic pain is increasing, we need more and better ways to treat pain. There are effective treatments for some causes and forms of pain, but we obviously have no magic medicine. Opioids remain as one of the most effective treatments for certain types of pain, but overuse of opioids can come at a cost at a societal and personal level. The use of cannabis for pain — either under the supervision of a health professional or as a personal choice — is another means by which patients are seeking different ways to address pain.
I think one very important result of chronic pain being recognized as a complex disease on its own is the increasing integration of multiple approaches for the treatment of pain, spanning from physical therapy, to psychological interventions, to lifestyle changes, to pharmaceuticals and so on. The effective treatment of pain is shifting to a broader patient-oriented approach, and the University of Toronto community is leading this movement.
What can webinar attendees expect from your remarks?
The objective of the webinar is to help increase awareness among the broader U of T community about pain and its impact on society. The University of Toronto Centre for the Study of Pain is a scientific hub of research that’s forging interdisciplinary links and developing bench to beside approaches to address pain.
Building on insights from our scientific community about the causes and effects of pain from molecules to communities, we will talk about how we can work to mitigate risk factors for chronic pain, and how we can engage the broader health community — including patients, physicians, pharmacists, and scientists — to improve pain treatment.
As a basic scientist, I will discuss what pain is at a biological level, why our brain receives signals to perceive different stimuli as painful, and how we use this knowledge to develop new tools and medicines to treat pain.
How can U of T’s Centre for the Study of Pain impact research and society?
The UTCSP is studying pain from a systems perspective, from the underlying mechanisms and biology of pain, to treatment options and how to mitigate risk factors in vulnerable populations. We have basic scientists working with clinicians across many health disciplines towards a shared goal of treating pain from a holistic perspective.
We also have a strong educational mandate to teach students in health professions about pain and to facilitate the career development of trainees in pain research. Pain is a broad problem that requires resources from many disciplines – the more we know, the more treatment options we can create that simultaneously helps patients, as well as address associated stigma and misinformation around chronic pain.
By engaging trainees in critical pain research, we’re training the next generation of health professionals and scientists who will can make breakthrough discoveries that will move science and health forward.
More News
Image

Pharmacy alum sees change in acceptance of Indigenous cultures in health care
During Deborah Emery’s 40-year pharmacy career, she provided care in Sioux Lookout, Thunder Bay and Manitoulin Island.
Read More
Image
Grad to Watch: Jackie Fule Liu’s research focuses on better outcomes for diabetes patients
A recent PhD graduate, Jackie Fule Liu combines hands-on skill and big-picture thinking to help tackle diabetes care challenges.
Read More
Image

U of T community members recognized with Order of Canada
Congratulations to Dean Emeritus and Professor K. Wayne Hindmarsh on his appointment.
Read More